
Will your job disappear?
July 30, 2025 Chris Rose PhD
Microsoft’s 2024 Copilot-chat study doesn’t give a countdown clock, but it does show how much of each occupation’s workload is already being done—successfully—by an LLM. That “AI-applicability” score is the best proxy we have for when displacement pressure could start:
- ≥ 0.40 Tasks are routinely completed by Copilot today. If employers decide to substitute AI for people, the impact could arrive within the next hiring cycle or two ( ≈ 1-3 years).
- 0.15 – 0.39 AI can help but not yet replace whole job bundles; think gradual erosion over 3-5 years as tools mature.
- ≤ 0.10 Little overlap with LLM abilities; jobs stay safe until robotics or other tech advances—5 + years out or longer.
Business choices ultimately control the pace; higher productivity could mean fewer staff—or simply higher ambitions with the same staff.
| Occupation / Category | AI-Applicability Score | Take-away | Earliest Pressure |
|---|---|---|---|
| Interpreters & Translators | 0.49 | Large share of translation, summarization, dialog handled natively by LLMs. | 1-3 yrs |
| Writers & Authors | 0.45 | Drafting and rewriting already common Copilot tasks. | 1-3 yrs |
| Customer Service Reps | 0.44 | Answer scripts, troubleshooting flows produced by AI. | 1-3 yrs |
| CNC Tool Programmers | 0.44 | Code-generation and spec parsing automated. | 1-3 yrs |
| Major group: Sales & Related | 0.32 | Pitches, FAQs, follow-ups drafted by AI; human relationship work remains. | 3-5 yrs |
| Office & Admin Support | 0.29 | Docs, minutes, data-entry steadily shifting to Copilot. | 3-5 yrs |
| Computer & Mathematical | 0.30 | Code scaffolding and data summaries aided, not fully automated. | 3-5 yrs |
| Low-impact examples: Nursing Assistants, Roofers, Dishwashers | < 0.10 | Work is physical, patient-facing, or messy—LLMs don’t do it. | 5 + yrs |
What this means for workers
- Knowledge and communication roles—especially those heavy on writing, explaining, or data look-ups—face the fastest automation pressure. These tasks are already demonstrated in live Copilot chats.
- Hands-on and care jobs remain largely insulated until AI systems gain reliable physical capabilities.
- Wages offer no shield: the correlation between pay and AI exposure is practically zero.
Bottom line: if your daily work is screen-bound and sentence-based, start planning for a future where a chunk of it is handled by a tireless text engine—and sooner rather than later. If it’s tool-belt, ladle, or stethoscope territory, you likely have more runway.
What if the fastest way to age a body isn’t a gene, a habit, or even time itself— but something that happened before you turned 18?
June 13, 2025 Chris Rose PhD

4 + Adverse Childhood Experiences (ACEs) = up to 20 fewer years of life-expectancy. Childhood trauma over-activates stress biology, accelerating heart disease, cancer, dementia and frailty decades later.
What we should do:
1. Integrate trauma into ageing research
Add validated ACE questionnaires + cortisol/epigenetic stress markers to every cohort and map the chain from early adversity → hallmarks of ageing → disease.
2. Translate fast
Fund trauma-buffering programs (such as parent coaching, stable housing, and stress-regulation training) with the same urgency as senolytics. This would be a cost-effective and evidence-based measure.
3. Advocate upstream
Develop policies that reduce poverty, guarantee paid family leave, and ensure mental-health parity are powerful population-level longevity tools, each capable of adding more disability-free years than any single late-life pill.
4. Model trauma-informed culture
Whether we’re in labs, clinics, classrooms, or companies, building psychological safety, predictable schedules, and easy access to support is essential, because scientific credibility now demands social responsibility—protecting tomorrow’s health-span begins today.
Your turn: What one policy or practice would you put in place to make trauma-informed care the norm? Drop your idea below
hashtag#ACEStudy hashtag#TraumaInformedCare hashtag#HealthyAging hashtag#HealthSpan hashtag#LongevityScience
The Golden Fountain of Youth
May 10, 2025
It’s 6:17 a.m. on a bleary Monday and you’re shuffling to the bathroom, half-convinced the universe should issue coffee via intravenous drip. You relieve yourself, flush, and lumber away—unaware you’ve just discarded a miniature cellular start-up capable of rebuilding cartilage, patching ulcers, or churning out therapeutic nanoparticles. That’s right: your morning pee is secretly littered with urine-derived stem cells (USCs)—the Marvel superheroes of the epithelial world, but minus the spandex(Zhou et al., 2011).
How on Earth did stem cells end up in pee?
Blame nature’s habit of cutting corners. The kidney’s plumbing sheds a few resilient progenitor cells each day. Most swirl away to oblivion; a brave minority survives the journey unscathed. Give those stowaways a Petri dish, some growth factor cocktails, and a warm incubator, and they reveal a party trick: divide like accountants on deadline and shapeshift into bone, fat, muscle, cartilage—basically the biological equivalent of a Swiss Army knife(Ji et al., 2017).
Scientists, displaying their signature flair for naming miracles, settled on “USCs,” In less than three weeks an expanded colony of these USCs can provide enough stem cells for systemic infusions, local injections, or Extracellular vesicles AKA EVs(Shi et al., 2025).
All from liquid waste you normally blame on last night’s asparagus.
Clinicians are intrigued because urine-derived stem cells offer needle-free sourcing—no bone-marrow drills or liposuction cannulas, just a sterile cup and a diligent lab tech—while still delivering fully personalized, autologous cells that leave the immune system unruffled; yet excitement is tempered by the “regulation reality check,” since any plan to reinfuse those cells triggers rigorous cell-therapy rules, complete with pathogen screens, karyotype audits, and enough paperwork to throttle Wi-Fi.
Final flush-worthy thought
Tomorrow morning, when biology calls, remember: the swirling liquid below isn’t just waste—it’s a disposable biobank with legitimate regenerative swagger. Capture it, culture it, and you might just grow the ingredients for your own personal tune-up. Or simply marvel at the fact that evolution lets priceless cells exit the body in the least glamorous way imaginable.
Ji, X., Wang, M., Chen, F., & Zhou, J. (2017). Urine-derived stem cells: The present and the future. In Stem Cells International (Vol. 2017). Hindawi Limited.
Shi, S., Zhu, C., Shi, S., Li, X., Muhammad, I., Xu, Q., Li, X., Zhao, Z., Liu, H., Fu, G., Song, M., Huang, X., Wang, F., & Cai, J. (2025). Human spindle-shaped urine-derived stem cell exosomes alleviate severe fatty liver ischemia–reperfusion injury by inhibiting ferroptosis via GPX4. Stem Cell Research and Therapy , 16.
Zhou, T., Benda, C., Duzinger, S., Huang, Y., Li, X., Li, Y., Guo, X., Cao, G., Chen, S., Hao, L., Chan, Y. C., Ng, K. M., Ho, J. C., Wieser, M., Wu, J., Redl, H., Tse, H. F., Grillari, J., Grillari-Voglauer, R., … Esteban, M. A. (2011). Generation of induced pluripotent stem cells from urine. Journal of the American Society of Nephrology, 22, 1221–1228.
Whispering Youth: FGF21’s Secret to Delaying Immune Aging
November 20, 2024
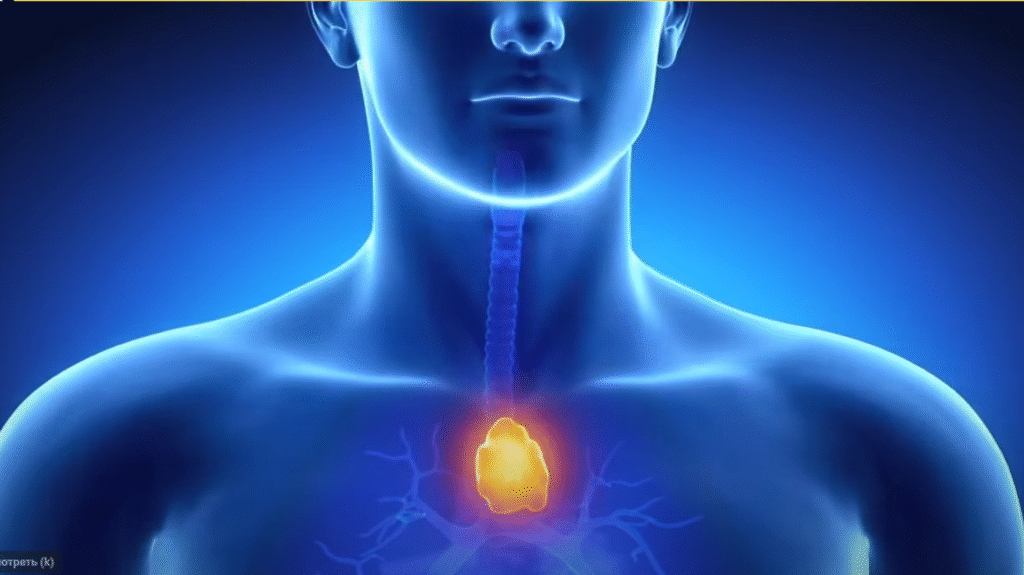
In the April 2025 issue of Nature Aging, first author Yun-Hee Youm and senior author Vishwa Deep Dixit report that simply raising blood levels of the hormone FGF21 does nothing to stop the thymus from shrinking and filling with fat in old mice. Instead, by genetically wiring thymic epithelial cells and the infiltrating adipocytes within the gland itself to produce FGF21 locally, they preserved the thymus’s structure, kept naïve T cells streaming into the bloodstream, and—even at 24 months—saw improvements in grip strength and motor coordination, classic signs of delayed immunosenescence.
To move this from mice to people, you’d need to:
- Choose a human-safe FGF21 platform (a long-acting protein analogue or a gene-therapy vector).
- Deliver it directly to the thymus (using TEC- or adipocyte-targeted vectors or ex-vivo–engineered cell grafts).
- Test in large animals to confirm local action, immune benefits, and absence of off-target effects.
- Establish noninvasive markers (imaging or blood assays) for thymus size, fat content, and naïve T-cell output.
- Run clinical trials—Phase I (safety), Phase II (proof of immune boost), Phase III (broad efficacy).
- Scale up manufacturing and satisfy regulators for your chosen biologic or vector.
- Define the ideal candidates and timing (e.g., older adults or patients with therapy-induced thymic damage).
Realistically, any single therapy built on this mouse model has barely a 1 percent chance of making it to the clinic—but with dozens of labs and companies racing to deliver pro‐thymic signals (from FGF21 analogues and IL-7 to mRNA platforms and biomaterials), the odds that one of these complementary approaches will ultimately succeed rise into the tens of percent over the next decade. That collective momentum gives real reason for cautious optimism
With that roadmap in place, we could one day coax our own thymus to sustain youthful immune function well into later life.
